-
Viewpoint on 'IONS'
Viewpoint on 'Scientific Literacy'
- Proudly sponsored by
-
-
Images Worth a Thousand... Birefringent Molecules
An image is worth a thousand words when describing complex physical phenomena; a recently developed technique can now help us actually picture birefringent fluids at the nanoscale.
-
Quantum Randomness on a Chip
A new approach to the generation of random numbers based on quantum optics may soon allow for safer online banking, e-commerce and data protection by efficiently generating truly random numbers.
-
A Brighter Summer under the Ice

While Venice and other coastal cities around the world are slowly sinking, during the Arctic summer the waters underneath the ice become brighter and brighter. Are these two scenarios connected to the continuous thinning of Arctic ice?
Volume 16 Story 4 - 25/1/2012
Now also in Spanish
El semáforo para la quimioterapia
and Portuguese
Semáforos para a quimioterapia,
brought to you by
Optics and Photonics Latin America
Despite medical progress, cancer is still a leading cause of death worldwide, with one in every three people being affected by the disease at some point in their lives. Chemical drugs are inherent in chemotherapy, itself one of the most effective ways to fight cancer. These chemicals, while aimed at killing fast-growing cancer cells, also harm healthy tissues, producing side effects such as infections, nausea, and hair loss. It is, therefore, desirable to recognize, as soon as possible, those patients for whom the benefits of chemotherapy outweigh the downsides. Thanks to a recent study carried out by Darren Roblyer, Bruce Tromberg and colleagues at the University of California, USA, it may one day be possible to know in which patients chemotherapy is effective, as early on as the very first day of treatment.
Roblyer, Tromberg and coworkers’ study focuses on women with breast cancer. In this case, chemotherapy is one of the most effective treatments available to shrink the size and reduce the grade of the tumor, leading to a more conservative breast surgery [1,2]. Between 8% and 20% of diagnosed women with breast cancer will, however, not show any progress, even after months of chemotherapy [1,3]. Therefore, knowing the likely response to chemotherapy in the early stages of cancer is of crucial importance for physicians to rapidly adapt the treatment before it is too late.
However, how is it possible to know from as early on as possible whether chemotherapy is effectively attacking the cancer cells? One way is by checking whether the tumor initiates an inflammatory response to recover from the damage inflicted by the chemotherapy. When a tissue suffers an injury with some cell damage, the body rapidly begins a healing process that starts with an acute inflammatory response, recruiting to the tissue more resources from the body by dilating the blood vessels to increase the blood flow. This kind of inflammatory response is what Roblyer, Tromberg and colleagues believe they are observing in tumors treated with chemotherapy. They used a technique called Diffuse Optical Spectroscopic Imaging (DOSI), which takes images of the tissue below the surface of the breast. DOSI can measure the concentration of various molecules in the blood by measuring how light of various colors gets scattered. In this study, the researchers measured the concentration of oxyhemoglobin, that is, hemoglobin saturated with oxygen, thus supplying the bloodstream with oxygen.
Surprisingly, in patients that responded to chemotherapy, the researchers observed an acute increase in oxyhemoglobin after only one day of treatment. This increase in oxyhemoglobin is thought to be due to an inflammation of the cancer cells that were effectively harmed and destroyed as a result of chemotherapy in responding patients. In this way, it was possible to distinguish between patients that responded positively, and patients that exhibited no beneficial response. "We were looking for early markers that would show us which patients should be receiving chemotherapy and which patients should be withdrawn from treatment with chemotherapy," Roblyer recalls, "but the results that we found were completely unanticipated."
According to Tromberg, DOSI could be used in the future, not only "to determine non-responding patients quickly and move on to surgery or other forms of treatment, but also as a way of guiding combined interventions, adding other adjuvant pharmaceutical agents to enhance inflammation and vascular reactivity for a better therapeutic effect." Indeed, this technique seems to have the potential of becoming a bedside test, allowing the monitoring of tumor progression in patients as frequently as desired. A National multi-center clinical trial supported by the American College of Radiology Imaging Networks (ACRIN) and the National Cancer Institute (NCI) is currently underway to evaluate DOSI technology.
According to Brian W. Pogue from Dartmouth College, USA, "the observation that vascular changes occur within one day of initiation of chemotherapy is exciting," because there is a compelling need for fast and cost-effective techniques to assess the patients’ response to chemotherapy. "As the number of options for therapy grows," Pogue adds, "and also as the recognition of individuality of response grows, it is critical to make choices about individuals during the course of therapy." Wei Yang from the University of Texas, USA, also shares the same enthusiasm: "If the results in this paper are validated in large prospective multicenter trials, there may be an impact on the selection of therapy to make personalized cancer therapy a reality." By taking advantage of these new developments, more effective treatment procedures could be implemented, potentially improving the quality of life and disease-free survival of breast cancer patients.
[1] P. Rastogi et al., Preoperative chemotherapy: Updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27, J. Clin. Oncol. 26, 778-785 (2008).
[2] J. R. Gralow et al., Preoperative therapy in invasive breast cancer: Pathologic assessment and systemic therapy issues in operable disease, J. Clin. Oncol. 26, 814-819 (2008).
[3] A. S. Caudle et al., Predictors of tumor progression during neoadjuvant chemotherapy in breast cancer, J. Clin. Oncol. 28, 1821-1828 (2010).

Traffic Lights for Chemotherapy
Many cancer patients do not respond to chemotherapy and have to endure harmful side effects even when the treatment itself does not prove effective. A new technique could, as of the very first day, give the green or red light to continuing with the treatment.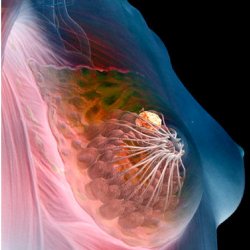
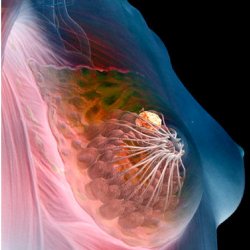
Breast cancer. The yellow mass in the illustration depicts a tumor located in a glandular tissue of the breast.
El semáforo para la quimioterapia
and Portuguese
Semáforos para a quimioterapia,
brought to you by
Optics and Photonics Latin America
Despite medical progress, cancer is still a leading cause of death worldwide, with one in every three people being affected by the disease at some point in their lives. Chemical drugs are inherent in chemotherapy, itself one of the most effective ways to fight cancer. These chemicals, while aimed at killing fast-growing cancer cells, also harm healthy tissues, producing side effects such as infections, nausea, and hair loss. It is, therefore, desirable to recognize, as soon as possible, those patients for whom the benefits of chemotherapy outweigh the downsides. Thanks to a recent study carried out by Darren Roblyer, Bruce Tromberg and colleagues at the University of California, USA, it may one day be possible to know in which patients chemotherapy is effective, as early on as the very first day of treatment.
Roblyer, Tromberg and coworkers’ study focuses on women with breast cancer. In this case, chemotherapy is one of the most effective treatments available to shrink the size and reduce the grade of the tumor, leading to a more conservative breast surgery [1,2]. Between 8% and 20% of diagnosed women with breast cancer will, however, not show any progress, even after months of chemotherapy [1,3]. Therefore, knowing the likely response to chemotherapy in the early stages of cancer is of crucial importance for physicians to rapidly adapt the treatment before it is too late.
However, how is it possible to know from as early on as possible whether chemotherapy is effectively attacking the cancer cells? One way is by checking whether the tumor initiates an inflammatory response to recover from the damage inflicted by the chemotherapy. When a tissue suffers an injury with some cell damage, the body rapidly begins a healing process that starts with an acute inflammatory response, recruiting to the tissue more resources from the body by dilating the blood vessels to increase the blood flow. This kind of inflammatory response is what Roblyer, Tromberg and colleagues believe they are observing in tumors treated with chemotherapy. They used a technique called Diffuse Optical Spectroscopic Imaging (DOSI), which takes images of the tissue below the surface of the breast. DOSI can measure the concentration of various molecules in the blood by measuring how light of various colors gets scattered. In this study, the researchers measured the concentration of oxyhemoglobin, that is, hemoglobin saturated with oxygen, thus supplying the bloodstream with oxygen.
Surprisingly, in patients that responded to chemotherapy, the researchers observed an acute increase in oxyhemoglobin after only one day of treatment. This increase in oxyhemoglobin is thought to be due to an inflammation of the cancer cells that were effectively harmed and destroyed as a result of chemotherapy in responding patients. In this way, it was possible to distinguish between patients that responded positively, and patients that exhibited no beneficial response. "We were looking for early markers that would show us which patients should be receiving chemotherapy and which patients should be withdrawn from treatment with chemotherapy," Roblyer recalls, "but the results that we found were completely unanticipated."
According to Tromberg, DOSI could be used in the future, not only "to determine non-responding patients quickly and move on to surgery or other forms of treatment, but also as a way of guiding combined interventions, adding other adjuvant pharmaceutical agents to enhance inflammation and vascular reactivity for a better therapeutic effect." Indeed, this technique seems to have the potential of becoming a bedside test, allowing the monitoring of tumor progression in patients as frequently as desired. A National multi-center clinical trial supported by the American College of Radiology Imaging Networks (ACRIN) and the National Cancer Institute (NCI) is currently underway to evaluate DOSI technology.
According to Brian W. Pogue from Dartmouth College, USA, "the observation that vascular changes occur within one day of initiation of chemotherapy is exciting," because there is a compelling need for fast and cost-effective techniques to assess the patients’ response to chemotherapy. "As the number of options for therapy grows," Pogue adds, "and also as the recognition of individuality of response grows, it is critical to make choices about individuals during the course of therapy." Wei Yang from the University of Texas, USA, also shares the same enthusiasm: "If the results in this paper are validated in large prospective multicenter trials, there may be an impact on the selection of therapy to make personalized cancer therapy a reality." By taking advantage of these new developments, more effective treatment procedures could be implemented, potentially improving the quality of life and disease-free survival of breast cancer patients.
[1] P. Rastogi et al., Preoperative chemotherapy: Updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27, J. Clin. Oncol. 26, 778-785 (2008).
[2] J. R. Gralow et al., Preoperative therapy in invasive breast cancer: Pathologic assessment and systemic therapy issues in operable disease, J. Clin. Oncol. 26, 814-819 (2008).
[3] A. S. Caudle et al., Predictors of tumor progression during neoadjuvant chemotherapy in breast cancer, J. Clin. Oncol. 28, 1821-1828 (2010).
Joana Braga Pereira
2012 © Optics & Photonics Focus
JBP is currently working on her Doctoral Thesis in Neuroimaging at the University of Barcelona, Spain.

Darren Roblyer, Shigeto Ueda, Albert Cerussi, Wendy Tanamai, Amanda Durkin, Rita Mehta, David Hsiang, John A. Butler, Christine McLaren, Wen-Pin Chen & Bruce Tromberg, Optical imaging of breast cancer oxyhemoglobin flare correlates with neoadjuvant chemotherapy response one day after starting treatment, PNAS (2011) 108, 14626–14631 (link).